How to Cover Coronavirus Surprise Bills
- Mar 31, 2020
- 4 min read
Updated: Apr 7, 2020
by Al Lewis
The short version of the story: you can actually save money by covering 100% all bills for all corona treatments up to 2x Medicare. But only if you give employees Quizzify’s surprise bill Prevent Consent and teach them how to use it to cap their/your total financial consent for emergency treatment at 2x Medicare. Otherwise 100% coverage could cost a lot of money.
For employees who use this surprise bill “Prevent Consent,” 100% coverage will then cost you less than standard coverage without the Prevent Consent.
And now, for the rest of the story
Seems like ancient history, but before coronavirus, the big healthcare news was surprise billing. The statistics were quite compelling. 57% of commercially insured Americans report having received one, for example.
While we are now best known for our coronaquizzes, played probably 100,000 times to date, it was our solution to surprise billing for emergencies that, to use the cliché-du-jour, went viral, being featured in the New York Times last month.
How did we make the New York Times? Simple: we solved the problem of surprise bills for emergencies. Don’t believe us? Read the article and our links.
In most states, if you don’t think your employees are getting surprise bills, that’s not because the bills aren’t high. It’s because employee share is low, either due to a low deductible and co-pay, or due to having already reached their deductible and paying low co-insurance. Hence you don’t hear complaints.
Absent complaints, these bills are being quietly auto-adjudicated and paid. Like the dirt from the tunnel in The Great Escape being sprinkled around the Stalag, these surprise bill expenses are sprinkled throughout your total spend. You wonder why you spend so much money in total, so you sort your spending every which way -- except this one: the multiple of Medicare for out-of-network providers in in-network facilities. That’s where these surprises are lurking.

Further, because elective care utilization (where our solution does not apply) has trended way down, your total spend may be artificially depressed this year. That makes you even less likely to notice these surprise bills for emergencies.
Surprise bills and coronavirus
Many insurers are waiving out-of-pocket fees for coronavirus treatment. Who do you think ends up paying for that waiver? Hint: it rhymes with “you.” Have you tracked health insurance stock performance lately? Far outperforming the market, kind of the opposite of what you would expect, right?
As an ERISA plan, you don’t have to go along with your carrier’s policy for corona coverage, but most of you are or will be.
This sets you up for the worst kind of surprise bill: one where the employee doesn’t complain. (See the previous section.) Therefore, you have no idea the bill even happened.
Surprise bills: now more than ever
Our solution works. It has been reported publicly twice, and privately to us several more times. It is right here. And it has never been more relevant than now, as this BenefitsPro article describes.
The reason for the increased relevance is that while our solution applies only to emergency admissions, visits, deliveries and transfers (and not to elective care), most medical care today fits those categories.
Since the majority of surprise bills involve those categories, surprise medical billing is now front-and-center. And as that BenefitsPro article described, employees are almost as fearful of the financial consequences of coronavirus as they are of the disease itself.
Whether or not you or your insurer have arranged special coverage for treatment, someone is paying for it. Therefore, your only option to avoid being hosed is to teach employees to use the Quizzify Prevent Consent. The optimal solution: offer full coverage to employees, and only to employees, who use it.
Even if you offer full coverage for corona, there is still the good chance that someone who is sick, after corona is ruled out, will be given treatment for something else. And out-of-pocket employee cost for that “something else” – under a non-corona diagnosis code – wouldn’t be covered. A surprise bill gobsmacking employees could be the result, absent this card.
Simple steps to make this happen
We are making this 100% coverage absurdly easy. As with our coronavirus resources, the basic resource is free. Your employees can access our surprise bill Prevent Consent three ways. The language is brief but effective, and is explained in detail here.
First, they can download the consent right into their Apple Wallets as an Apple Pass. Here is what their Apple Wallet might look like if they download this Pass (and some of our other Passes), with the language right in it:

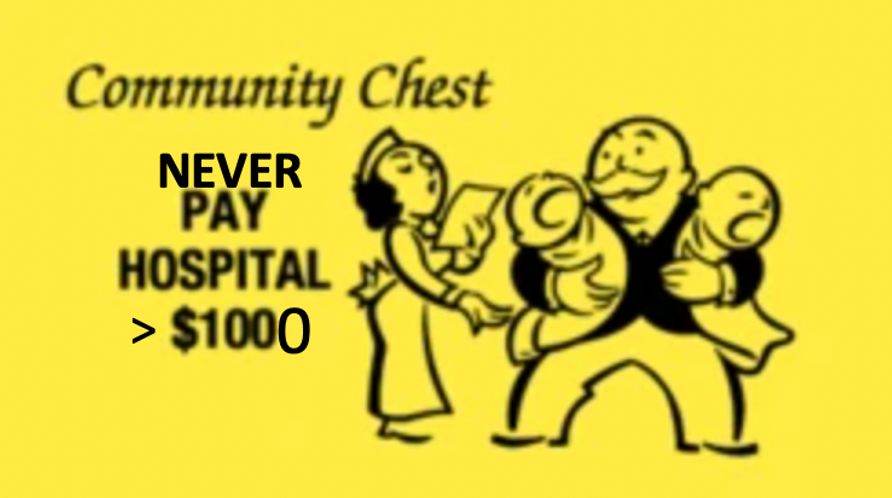
Second, you or they can download a sheet with eight paper cut-outs on it, to be placed strategically in employee houses, cars, bicycles, motorbikes etc., that look like this (only showing 4, but you get the point):

Third, if you can send a stamped-self-address envelope to us at 37 Pennsylvania Avenue, Newton MA 02464, we will send you gratis the language on transparent tape to affix to insurance cards, as well as actual cards, with our information on the back in case someone gives your employees a hard time and we need to do some explaining.
We will send some for personal use gratis. If you want more, please throw in a few dollars, as these were not free to produce.
As an example of the transparent tape, here is our Quizmeister-in-Chief’s insurance card…

And here is the actual, signable card itself, that he carries with him:

Next steps to create this win-win should be very clear: cap spending for emergencies while providing 100% coverage to employees who use the card.

Quizzify provides the education employees need to be health-literate, wiser and more confident healthcare consumers
Teach employees how to navigate the ins and outs of their health benefits and gain valuable information about better health practices. With quizzes reviewed by doctors at Harvard Medical School, Quizzify helps employees live healthier lives and save money on healthcare... without collecting any private health information.
Benefits are of no value if employees don’t use them. You can customize Quizzify so that your quiz questions can explain exactly what the value is...and our “learn more” links can point employees to exactly where they need to go.